Think of some of the ways you sit. Whether taking a ride on the subway, waiting patiently at the doctor’s office, or sitting as a passenger in a car, the way we sit, especially for prolonged periods can have an effect on the pain we may experience in our low back.
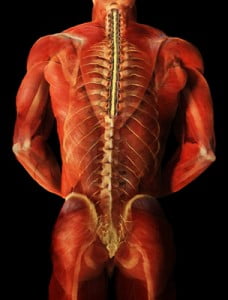
For many of us, sitting with our legs crossed feels comfortable in the moment but have you ever considered how this can affect your back and cause pain? What happens to your spine and muscles when sitting with your legs crossed for an extended period of time? When considering good posture, a large component is keeping your spine neutral and avoiding positions that twist the spine or cause misalignment. When sitting with your legs crossed, your pelvis becomes tilted and unconsciously, we tilt our entire torso towards one side. There is a curvature towards one side in the low back which then creates problems in other areas of the spine. Naturally, with a tilt of the pelvis, the upper body will compensate by leaning the opposite direction to maintain balance. Working from the bottom up, pressure on the lumbar spine will cause curvature and misalignment in the thoracic spine. This places strain on the cervical spine to keep the head in the upright position.
Sitting with our legs crossed can also affect our muscles. There are two common sitting positions that we should be mindful of, knee over knee or foot over knee for a prolonged period can cause a tightness in the hamstrings, hip flexors and glute muscles. The iliopsoas, one of the major hip flexor muscles, is responsible for external rotation of the femur and an integral part in maintaining posture. This muscle may become strained due to contraction while the pelvis is tilted. You may notice soreness and tenderness in the low back and hip area. Similarly, sitting foot over knee can over time damage the muscles in the inner thigh. Most commonly, the sartorius muscle can become tight and cause discomfort when sitting with the calf over the knee. At the Norman Marcus Pain Institute, Iliacus and Psoas muscles on the hip can be treated for pain. As one of the most common muscles causing pain for patients, when treated, the Iliacus and other hip flexors can provide great relief for pain in the low back, buttock and groin.
Instead of sitting with crossed legs, sit in a chair with height necessary to place both feet flat on the floor. While sitting upright with your back against the chair, you may want to consider placing a cushion under your bottom that can add support to the low back.
References
Lee BJ, Cha HG, Lee WH. The effects of sitting with the right leg crossed on the trunk length and pelvic torsion of healthy individuals. J Phys Ther Sci. 2016 Nov;28(11):3162-3164. doi: 10.1589/jpts.28.3162. Epub 2016 Nov 29. PMID: 27942141; PMCID: PMC5140821.




 grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.

