This excerpt from my book End Back Pain Forever, is about my mentor and friend, Dr. Hans Kraus. He changed the way I viewed pain and the treatment of pain, and enhanced my life and ultimately my patients’ lives for the better.
Chapter 2
You Are Not Alone: The Back Pain Epidemic (Part 4)
Then, in 1993, I met Dr. Hans Kraus. He was to transform my life and the life of my patients. He was eighty-five years old and had just retired from his practice as a specialist in physical medicine and rehabilitation. He had also given up mountaineering and rock climbing. In all those pursuits, he had won international acclaim. Originally trained as an orthopedic surgeon at the University of Vienna, Dr. Kraus was well known for having successfully treated President John F. Kennedy’s back after all prior treatments had failed. Yet his nonsurgical approach to treating patients with muscle pain, especially low back pain, was not accepted by other doctors, including some of the very doctors who referred their own patients to him for what proved to be successful treatment.
For example, one prominent orthopedic surgeon at the Columbia University School of Medicine, Dr. Frank Stinchfield, who routinely sent many of his back pain patients to Dr. Kraus, underwent spinal surgery rather than consult him for his own back pain after a herniated disk was diagnosed. The surgery failed, and Dr. Stinchfield was never able to work again because of unrelenting pain.
Another disappointing example was that of Dr. Jonas Salk, best known for developing the first safe and effective polio vaccine. Dr. Salk did consult Dr. Kraus for back pain, and the treatment was successful. It eliminated Dr. Salk’s pain and allowed him to avoid surgery. Yet when Dr. Kraus needed Dr. Salk’s help to obtain research support, the famed medical researcher declined. He said that muscle pain didn’t have a “scientific foundation.” That has since changed, and we will look at the basic research explaining the mechanisms of muscle pain in Chapter 4.
In our first meeting, Dr. Kraus asked what I did. I told him that I treated patients with chronic pain.
“How do you do that?” he asked.
“I teach them how to manage their pain, how to deal with it, live with it.”
“Why not get rid of their pain?”
“Because it’s chronic pain,” I said. “You can sometimes reduce it, but you can’t get rid of it.”
He persisted. “Have you treated the muscles?”
“We treat the muscles with aerobic exercises.”
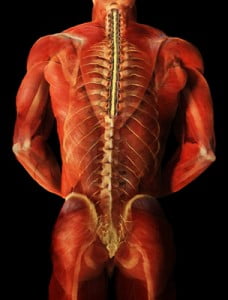
“Aerobic exercises? Really? Muscle pain caused by muscle spasm, tension, stiffness, and trigger points does not respond to aerobics. But it will respond to other types of exercises: prescribed exercises designed to treat the specific source of pain. That’s what I’ve done.”
“Low-impact aerobics are the standard way,” I said.
“They may be the standard way,” he replied. “But they are sure to make many of your patients feel worse.”
He asked if I had “very difficult cases,” and I told him that I did. “Some,” I added, “are impossible to treat.”
“Would you mind if I were to examine one of them?”
——————————————————————————————————————————————–


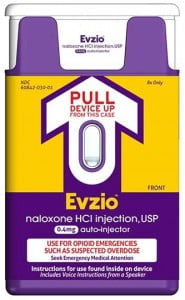
 Some opioids, such as oxycodone, are often combined with Tylenol (
Some opioids, such as oxycodone, are often combined with Tylenol (
