Monday, February 17th, 2014 at
9:30 AM
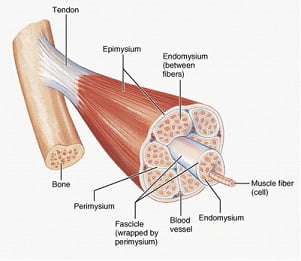
The most common method in treating trigger points is with trigger point injections. Simply put, trigger point injections are needles being placed into the taut, tender points of the muscle. However, there are different techniques in injecting the muscle fibers.
There are two major types of needles used in injecting the muscle. With dry needling, it is common to use acupuncture needles[1], which are small, thin and flexible. When a liquid is injected in the muscle (such as saline or lidocaine), hypodermic needles are used, which is a hollow needle that is generally thicker and is not flexible.
Different fluids (injectates) can be used in trigger point injections. Lidocaine or bupivacaine are commonly used, which are numbing agents. Corticosteroids and botulinum toxin (better known as Botox) are also used, in hopes that the injectate would reverse the changes in the trigger point rather than just the needle causing minor damage and inflammation which is thought to lead to regrowth of normal muscle fibers. Still others have used saline. Studies have shown that it didn’t matter what was injected into the muscle[2]; there was not a noticeable difference in pain relief between the different injected substances. Also, dry needling injections seem to be just as effective as injections with any substance, suggesting that what is injected is not what causes relief but rather the physical needling of the muscle.
Other treatments used for trigger points include:
-TENS (transcutaneous electrical stimulation) – electrodes are applied to the skin, sending an electric current to the nerves in the skin. The nerves then transmit a signal to the brain. This signal is competing with the signal coming from your painful area. So, instead of feeling your normal pain, you’ll feel a buzzing sensation where the electrodes are attached.
-“spray and stretch” – a technique in which ethyl chloride spray (or a comparable cold) is used to numb a painful area, followed by gentle stretching
-ultrasound
-low level laser
The fact that so many different approaches claim to be effective indicates that there is confusion concerning the understanding and treatment of pain thought to be coming from trigger points. All muscle pain is not caused by trigger points. My associates and I discuss the need for a comprehensive approach to muscle pain in a study published in Pain Medicine[3]. (This article can be accessed here.
[1] Mense, Siegfried, and Robert Gerwin. Muscle Pain: Diagnosis and Treatment. Heidelberg: Springer, 2010
[2] Cummings, T.Michael, and Adrian R. White. “Needling Therapies in the Management of Myofascial Trigger Point Pain: A Systematic Review.” Archives of Physical Medicine and Rehabilitation 82.7 (2001): 986-92.
[3] Marcus, Norman J., Edward J. Gracely, and Kelly O. Keefe. “A Comprehensive Protocol to Diagnose and Treat Pain of Muscular Origin May Successfully and Reliably Decrease or Eliminate Pain in a Chronic Pain Population.” Pain Medicine 11.1 (2010): 25-34.