Dr. Marcus learned about the importance of muscles from his mentor, Dr. Hans Kraus. Dr. Kraus taught Dr. Marcus how to examine the body for muscle pain and how he treats each muscle. Dr. Kraus was known as one of the fathers of sports medicine. He is also known for having treated President John F Kennedy’s back pain.
Archive for 'muscle pain'
Dr. Hans Kraus – Mentor to Dr. Marcus
How important is your diagnosis?
 I met a lovely 53 year old gentleman, who was suffering from severe low back and hip pain for over a year, diagnosed with a herniated disc. He had tried physical therapy with some relief, but still was unable to eliminate his pain. After diagnosing and treating muscles in his low back, buttock, and thigh, he reported no low back pain, and was discharged from our office. However, after five years, he returned to our office, stating that he had foot pain, diagnosed with plantar fasciitis, and unable to rock climb or hike without severe pain in his calves and feet. After identifying and treating multiple muscles in his calves, shins, and feet, he reported 100% relief, and even finished a 10 day rock climbing trip. Although you may be given one diagnosis, sometimes we find muscle involvement and are able to eliminate the pain!
I met a lovely 53 year old gentleman, who was suffering from severe low back and hip pain for over a year, diagnosed with a herniated disc. He had tried physical therapy with some relief, but still was unable to eliminate his pain. After diagnosing and treating muscles in his low back, buttock, and thigh, he reported no low back pain, and was discharged from our office. However, after five years, he returned to our office, stating that he had foot pain, diagnosed with plantar fasciitis, and unable to rock climb or hike without severe pain in his calves and feet. After identifying and treating multiple muscles in his calves, shins, and feet, he reported 100% relief, and even finished a 10 day rock climbing trip. Although you may be given one diagnosis, sometimes we find muscle involvement and are able to eliminate the pain!
Ehlers-Danlos Syndrome (EDS) Demographics & Characteristics
A recent study released by Rheumatology takes a look at the demographics of 280 patients previously diagnosed with hypermobility syndrome. They gathered a cohort of 280 patients – 90% female and 10% male, between ages 18 and 66 (it is generally accepted that females have a higher rate of hypermobility than males, though it is not clear why). 95% of these patients had what was previously known as EDS type 3, now known as hypermobile Ehlers-Danlos Syndrome (hEDS). They proceeded to analyze a comprehensive medical history.
The average age of diagnosis of these patients was 29. 66% of patients had a family history of hypermobility, which corresponds with what we know about the genetic nature of Ehlers-Danlos syndrome. A family history of hypermobility and/or EDS is one of the accepted criteria to be diagnosed with hEDS.
66% of the patients had orthostatic intolerance, meaning their vitals changed dramatically when standing up and returned to “normal” when lying down. This includes drastic increases in heart rate and decreases in blood pressure due to the body’s inability to properly compensate for the challenges of standing upright. Almost half of those with orthostatic intolerance had bowel problems, compared to only 19% without intolerance. 45% had gastrointestinal problems, and 39% had bladder dysfunction. Chronic joint and muscle pain were reported in 91% of the patients. Approximately half of these patients with chronic pain used opioids long-term to relieve their pain. 43% patients reported being on work disability.
While the official clinical diagnoses for hypermobile EDS focus on joint hypermobility and skin hyperextensibility, the study confirms that this particular condition is systemic and also has a high correlation to orthostatic intolerance and chronic pain. Therefore it is important to look at a holistic, overall approach of each patient suspected to have hEDS in order to properly assess how to improve the quality of life of each person living with hEDS.
Ref: Dojcinovska, M., Cohen, H., & Wolman, R. (2019). 200 Demographics and clinical characteristics of a national cohort of 280 patients with hypermobility syndrome and impact on their work disability. Rheumatology, 58(Supplement_3), kez107-016.
Ehlers-Danlos (EDS)
It is known that physically active patients who have stiff muscles frequently develop pain. What is less known is that patients with overly flexible joints will also frequently develop muscle pain.
Congenital diseases, such as Marfan Syndrome and Ehlers-Danlos Syndrome (EDS), may cause joints to repeatedly dislocate, resulting in stiffness in the muscles surrounding the joint – a way that the body attempts to help the unstable joint. The reflexive stiffness and spasms in the muscles surrounding the unstable joint cause pain.
Treatment to relax the muscles such as injections into trigger points or into the muscle attachments may do too good a job – that is, if the muscles become too relaxed, the joint may become too loose and continue to dislocate.
An alternative treatment we have used is low level laser therapy (LLLT). LLLT uses light energy in a narrow wavelength (810-980nm) to deeply penetrate through the skin into the muscles and tendons. LLLT produces an increase in chemicals in the body (Cytochrome C Oxidase) that enables the production of ATP (adenosine triphosphate) which can aid in healing damaged tissue. Using LLLT to reduce pain in EDS patients has resulted in ~40% decrease in pain lasting for 3-4 weeks (or even longer!) without making the underlying muscle too loose.
Read more about EDS HERE
Is Looking Good Worth Having Back Pain?
There is an old expression, “beauty is pain.” Does it need to be? Is it worth risking your long-term health? Why do women wear high-heeled shoes when they know that looking beautiful in the moment may cause them pain down the road? Scientists from the Universite de Bretagne-Sud recently conducted experiments, which studied the effects of high-heeled women on men. Women who wore higher heels (3-4 inches vs. 2 inch heels) were able to get more men to answer survey questions on the streets and were picked up faster in bars and clubs. These studies show some type of empowerment in women with high-heeled shoes.  Knowing that this empowerment exists, and as fashion has increased the height of heels from 4 inches to 5 inches, we would like to remind you that walking for extended periods in high heels can cause calf tendons to shorten and possibly result in an increase in low back pain.
Knowing that this empowerment exists, and as fashion has increased the height of heels from 4 inches to 5 inches, we would like to remind you that walking for extended periods in high heels can cause calf tendons to shorten and possibly result in an increase in low back pain.
Here at the Norman Marcus Pain Institute, we see patients that run the gamut of factors causing their back pain. Prevention is always the best treatment; since low back pain affects so many of us a simple intervention is being more conscious of our shoes! While those Manolo Blahniks and Jimmy Choos may be stunning, they may be causing a problem for you down the line. At NMPI, we won’t say don’t wear them, just please, wear them in moderation.
Is Bad Weather To Blame For Your Lower Back Pain?
A New York Times article Weather May Not Affect Back Pain, printed mid-July, cited a study showing that weather may not affect back pain. The purpose of the study was to explore the often-heard complaint from patients diagnosed with persistent pain related to muscles and bones (musculoskeletal pain) that weather changes cause an increase in pain. The study was based on an analysis of 993 patients who had seen their physician in 2011-2012 complaining of an episode of sudden back pain. These were not patients with a history of back pain.
So this article does not actually examine patients who already have back pain to see if the pain is increased with bad weather. In my practice, at NMPI, I have patients who can tell me a snowstorm is coming 3 days before it occurs. Although studies of the association between weather and pain are not uniformly supportive of the connection, a study done in 1995 of 558 patients with chronic pain found that 2/3 experienced an increase in pain and most of them prior to the occurrence of the bad weather.
 I have patients whose pain is so severe with bad weather that they can hardly get out of bed. Although there is no good scientific explanation for this association, some suggestions have been offered. When the barometric pressure falls, the air pressure in a painful joint may continue to be a little higher than the air pressure on the outside of the body, causing an increase in pain. Another explanation is that cold and/or inclement weather decreases the amount of time you are outside and active. Patients with musculoskeletal problems (i.e. muscle pain and arthritis) often feel worse with inactivity. In addition cold weather causes the blood vessels in the hands and feet to constrict, which can decrease the amount of available oxygen, resulting in increased muscle pain.
I have patients whose pain is so severe with bad weather that they can hardly get out of bed. Although there is no good scientific explanation for this association, some suggestions have been offered. When the barometric pressure falls, the air pressure in a painful joint may continue to be a little higher than the air pressure on the outside of the body, causing an increase in pain. Another explanation is that cold and/or inclement weather decreases the amount of time you are outside and active. Patients with musculoskeletal problems (i.e. muscle pain and arthritis) often feel worse with inactivity. In addition cold weather causes the blood vessels in the hands and feet to constrict, which can decrease the amount of available oxygen, resulting in increased muscle pain.
If your history indicates that bad weather causes an increase in your pain, it is likely that your flare up is most likely not an indicator of physical deterioration. Additional pain can be reasonably treated with increased medication for the brief period of weather related pain.
Sometimes the pain isn’t coming from where you think
I recently saw Fred, a 30 year old male, who complained of significant neck pain and shoulder pain. The pain on his left side was much greater than on the right. He tried several chiropractic treatments, massage, physical therapy, acupuncture, and exercises without relief of his pain.
When I first examined Fred, I found two muscles that were painful, his anterior and medial scalenes on both sides. The scalenes are muscles that go from the side of the neck down to the 1st rib as it sits under the clavicle (collarbone). Since he complained mostly of pain on his left neck and shoulder, I injected his left scalenes, followed by 3 days of physical therapy (which included neuromuscular electrical stimulation and gentle, limbering exercises). Fred claimed that the pain on the left subsided, but he noticed that the right side was now more painful. So, the following week, he had his right scalenes treated (with injections into the muscle, followed by 3 days of physical therapy). Fred reported a significant decrease in his overall pain, and reported only soreness at the injection sites.
I followed up with Fred approximately one month later. He reported to me that his overall pain level continued to stay low, but he noticed that when he looked up, he felt tightness on the left side of his neck. When I examined him, I found two muscles to be contributing to his pain, the Serratus Anterior and the Subscapularis. These muscles are in his shoulder. He was very shocked to learn that tightness in his neck was caused by muscles in his shoulder!!
Once these muscles were treated, he reported that the tightness in his neck was released. Sometimes we have to look for muscles contributing to pain in areas other than where you may be feeling it. This is called referred pain. If I had continued to treat muscles in Fred’s neck, he may never have had relief!
Case Study: Low Level Laser Therapy
Gregory is a 29 year old manager whose job requires that he travel often. He came to see me for pain at the back of the left side of his neck which he often felt upon waking up, and during or after jogging over the past 4-5 years. An MRI showed that his neck did not have any significant spinal abnormalities that might be causing his pain, but a physical examination revealed three muscles that were likely the source of his pain.
I began treating Gregory with a 15 watt class 4 laser. On his second day of treatment, he reported that he felt no pain in the left side of his neck when he woke up, but that the pain had moved to the right side of the neck and shoulder. I continued treating the left side of his neck, and also began to treat the right side with the laser.
When he returned for the third day of treatment, the pain in the left side of his neck was completely gone, and the right side’s discomfort was significantly reduced. At a two month follow-up, his pain was gone.
He is now able to go jogging without any pain in his shoulders or neck. By starting with a conservative treatment approach, Gregory was able to avoid invasive or costly procedures, and regain function.
Treating trigger points in muscles
The most common method in treating trigger points is with trigger point injections. Simply put, trigger point injections are needles being placed into the taut, tender points of the muscle. However, there are different techniques in injecting the muscle fibers.
There are two major types of needles used in injecting the muscle. With dry needling, it is common to use acupuncture needles[1], which are small, thin and flexible. When a liquid is injected in the muscle (such as saline or lidocaine), hypodermic needles are used, which is a hollow needle that is generally thicker and is not flexible.
Different fluids (injectates) can be used in trigger point injections. Lidocaine or bupivacaine are commonly used, which are numbing agents. Corticosteroids and botulinum toxin (better known as Botox) are also used, in hopes that the injectate would reverse the changes in the trigger point rather than just the needle causing minor damage and inflammation which is thought to lead to regrowth of normal muscle fibers. Still others have used saline. Studies have shown that it didn’t matter what was injected into the muscle[2]; there was not a noticeable difference in pain relief between the different injected substances. Also, dry needling injections seem to be just as effective as injections with any substance, suggesting that what is injected is not what causes relief but rather the physical needling of the muscle.
Other treatments used for trigger points include:
-TENS (transcutaneous electrical stimulation) – electrodes are applied to the skin, sending an electric current to the nerves in the skin. The nerves then transmit a signal to the brain. This signal is competing with the signal coming from your painful area. So, instead of feeling your normal pain, you’ll feel a buzzing sensation where the electrodes are attached.
-“spray and stretch” – a technique in which ethyl chloride spray (or a comparable cold) is used to numb a painful area, followed by gentle stretching
-ultrasound
-low level laser
The fact that so many different approaches claim to be effective indicates that there is confusion concerning the understanding and treatment of pain thought to be coming from trigger points. All muscle pain is not caused by trigger points. My associates and I discuss the need for a comprehensive approach to muscle pain in a study published in Pain Medicine[3]. (This article can be accessed here.
[1] Mense, Siegfried, and Robert Gerwin. Muscle Pain: Diagnosis and Treatment. Heidelberg: Springer, 2010
[2] Cummings, T.Michael, and Adrian R. White. “Needling Therapies in the Management of Myofascial Trigger Point Pain: A Systematic Review.” Archives of Physical Medicine and Rehabilitation 82.7 (2001): 986-92.
[3] Marcus, Norman J., Edward J. Gracely, and Kelly O. Keefe. “A Comprehensive Protocol to Diagnose and Treat Pain of Muscular Origin May Successfully and Reliably Decrease or Eliminate Pain in a Chronic Pain Population.” Pain Medicine 11.1 (2010): 25-34.
What are trigger points?
Have you ever felt a painful tightness that just won’t go away no matter how much you stretch? Even if the pain subsides or goes away temporarily, when it recurs you still feel a tender knot that’s always in the same area. This may be due to trigger points (TrPs). TrPs are tender nodules which can cause pain and are found in a taut band of muscle tissue. This taut band is formed from a small group of contracted muscle fibers which will make that region of your muscle feel hard and tender. TrPs are sensitive to pressure and movement. Pressing on a trigger point will cause pain.
TrPs can be classified as either active or latent. A latent TrP is one that causes pain when palpated, or pressed on, but not spontaneously while resting. An active TrP can cause spontaneous pain – either at rest, in use, or while being pressed. If there is enough stress – for example, from too much exercise, a latent TrP can transform into an active TrP.
The cause of TrPs is still being studied, however, there is speculation that the taut band appears in the muscle first without any tenderness or irritation. With additional stress, the hardened area becomes tender to the touch (a latent TrP), and finally, may progress to producing spontaneous pain as an active TrP. The initial hardness in a band of muscle fibers can be caused my multiple factors: injury, overstretching, or over-exercising.
TrPs can be a debilitating source of pain. They can cause weakness and lack of coordination in the muscles where they are found. Next blog, we will discuss common treatment options for trigger points.
Muscles as the source of pain
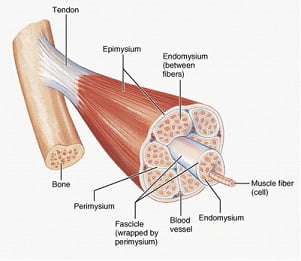
Muscles are the largest organ system in the body, accounting for approximately 50% of our body weight. We have different ways of categorizing muscles: how they look, how they move, and where they’re located. We are going to focus on muscles that move voluntarily, which means we tell the muscles to move, as opposed to involuntary muscles, which automatically move on their own (like our heart and blood vessels). There are 641 muscles in the body – 340 pairs (meaning we have one on the right, and one on the left), and one unpaired (which is the transverse arytenoid for those who must know).
70% of lower back pain is diagnosed as idiopathic or non-specific[1], which means we are not sure what caused the pain. However, most investigators believe that sprains and strains of the soft tissue are the source of pain. Soft tissue refers to muscles, tendons, and ligaments. So it may be surprising that the emphasis in evaluating and treating lower back pain, neck pain, and shoulder pain, is on the spine and the nerves coming out of the spine. In fact, from 1997 to 2005, the prevalence of the diagnosis of spine-related issues has increased 100% while the diagnosis of strains and sprains of soft tissue has gone down by 40%[2].
This is generally attributed to the increase in the use of high-tech imaging studies, such as MRI and CT scans. However, just because we have a clearer image of what’s going on inside of your body doesn’t mean that we have a clearer understanding of what’s causing your pain. More than 90% of lower spine MRIs exams in adults are abnormal[3]. Studies have found that up to 40% of people have herniated discs and as many as 70% have degenerated discs with no pain. If people can walk around with abnormal spines without pain, then this means that abnormalities in the spine aren’t always the cause of pain. Your diagnosis of a herniated disc, spinal stenosis, or spondylosisthesis may actually be unrelated to your source of pain.
Muscles are often ignored when it comes to diagnosing pain. I believe the reason is that we rarely evaluate muscles as a source of pain. We generally don’t learn about or understand how they work, what chemical changes take place inside, and how they produce pain (the pathophysiology). I would like to take the next few blogs to discuss how muscles contribute to your chronic pain.