Dr. Marcus learned about the importance of muscles from his mentor, Dr. Hans Kraus. Dr. Kraus taught Dr. Marcus how to examine the body for muscle pain and how he treats each muscle. Dr. Kraus was known as one of the fathers of sports medicine. He is also known for having treated President John F Kennedy’s back pain.
Archive for 'Dr. Norman Marcus'
Dr. Hans Kraus – Mentor to Dr. Marcus
Ehlers-Danlos (EDS)
It is known that physically active patients who have stiff muscles frequently develop pain. What is less known is that patients with overly flexible joints will also frequently develop muscle pain.
Congenital diseases, such as Marfan Syndrome and Ehlers-Danlos Syndrome (EDS), may cause joints to repeatedly dislocate, resulting in stiffness in the muscles surrounding the joint – a way that the body attempts to help the unstable joint. The reflexive stiffness and spasms in the muscles surrounding the unstable joint cause pain.
Treatment to relax the muscles such as injections into trigger points or into the muscle attachments may do too good a job – that is, if the muscles become too relaxed, the joint may become too loose and continue to dislocate.
An alternative treatment we have used is low level laser therapy (LLLT). LLLT uses light energy in a narrow wavelength (810-980nm) to deeply penetrate through the skin into the muscles and tendons. LLLT produces an increase in chemicals in the body (Cytochrome C Oxidase) that enables the production of ATP (adenosine triphosphate) which can aid in healing damaged tissue. Using LLLT to reduce pain in EDS patients has resulted in ~40% decrease in pain lasting for 3-4 weeks (or even longer!) without making the underlying muscle too loose.
Read more about EDS HERE
The Start of Baseball Season
The baseball season just opened and already players are calling off their first few games due to “tweaked knees” and “sore backs”. As the sun is starting to come out, and the snow is (FINALLY!) melting, many of us are anxious to get outside and start playing sports again. However, this is also a time where pain can start rearing its ugly head. Many people forget to limber and stretch properly before AND after playing sports, causing strains and sprains of muscles.
So keep in mind these important tips to get moving again this spring:
- Do gentle limbering stretches every day to help maintain flexibility of your muscles.
- Stretch before and after any exercise.
- Start slowly – if you haven’t moved all winter, start with simple exercises, like walking, before starting anything more difficult.
- If you’re feeling extremely sore the following day, it means you may have done too much. Cut back on the difficulty and amount of time the next time you exercise. Slowly increase the difficulty and the length of the session. A safe rule of thumb is to start out after a long layoff at 50% of your prior routine and then increase 15-20% every 5-7 days as long as you feel okay at any level before going to the next.
- Drink lots of water!
Is access to your medical records a good thing?
More and more doctors are transferring their records to an electronic format. One electronic medical records software, OpenNotes, allows patients to view their medical records online as well. Does having this information mean better care for a patient?
The New York Times published an article about one patient, Steven Keating, who benefited from the ability of seeing his medical records. In fact, because of this, he was able to push his doctors to perform an MRI of his brain, which revealed a brain tumor the size of a tennis ball.
In other cases, having this unfiltered information may create unne cessary concern and anxiety. For example, if one of your blood levels isn’t within the “normal range,” what does this mean? Most people would probably run to their computer and search “abnormal blood level for _________” and get countless different possible diagnoses….most of them serious, and probably not related to your “abnormal” blood levels. Results of imaging studies, such as x-rays and MRIs may also appear to be serious when they are actually only reflecting the results of age and normal wear and tear.
cessary concern and anxiety. For example, if one of your blood levels isn’t within the “normal range,” what does this mean? Most people would probably run to their computer and search “abnormal blood level for _________” and get countless different possible diagnoses….most of them serious, and probably not related to your “abnormal” blood levels. Results of imaging studies, such as x-rays and MRIs may also appear to be serious when they are actually only reflecting the results of age and normal wear and tear.
Just having raw data and unfiltered notes is not generally useful and can be harmful. If you are going to get your notes, make sure to discuss your concerns regarding what you read with your physician.
Acetaminophen
The BMJ (what used to be called the British Medical Journal) just published an article stating that acetaminophen (ie Tylenol) has been found to provide no relief in low back pain (compared to a placebo). Acetaminophen was also related to a risk of having an abnormal liver test. The article included data from 13 randomized controlled trials (RCTs).
An RCT to evaluate a drug is a research study where one group of people receives the actual drug (in this case, acetaminophen) and the other group receives a placebo (a pill with no active ingredient, generally a sugar pill). Then, data is collected from both groups to see if either achieved any pain relief. In this analysis, it shows that whether you receive acetaminophen or a sugar pill, you had the same amount of pain relief – meaning that active drug had no real pain relief effect.
relief. In this analysis, it shows that whether you receive acetaminophen or a sugar pill, you had the same amount of pain relief – meaning that active drug had no real pain relief effect.
Although most of the patients I see find no relief from acetaminophen, a small percentage of patients do, so don’t completely dismiss this drug when it comes to helping your pain. However, if you do take acetaminophen, make sure that you’re not taking too much. The FDA recommends taking less than 3000mg a day. This means if you’re taking Extra Strength Tylenol (500mg), you can only take 6 pills a day, or regular strength, 300mg, 10 pills a day. Higher amounts can lead to liver damage that could even be life-threatening.
Rafael Nadal will receive stem cell therapy for back pain – Should You?
Earlier in November, Rafael Nadal, the 14-time Grand Slam winner, announced he would receive stem cell treatment to help heal his ailing back, the same type of treatment he received for his knee. His doctor in Barcelona, Dr. Angel Ruiz-Cotorro, who has been treating Nadal for 14 years, said, “Nadal’s back pain is ‘typical of tennis’ players in that the treatment is meant to help repair his cartilage.” Stem cells were recently extracted from Nadal for a cultivation process to “produce the necessary quantities,” said Ruiz-Cotorro. Once cultivated, the stem cells will be placed into the joints of his spine with the goal of regeneration of cartilage as well as for an anti-inflammatory effect. Dr. Ruiz-Cotorro predicts that Nadal can return to training in early December.
Will stem cell treatment work for Nadal’s Back Pain?
Stem cell treatment may seem logical in certain situations – for example, if you have a mechanical problem where a knee has worn out cartilage, causing bone to rub against bone, it makes sense to use stem cells to grow new cartilage to have a cushion to protect the bone and cause the knee to be less painful. As much as we may want to see him back on the courts  grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
grabbing more grand slam titles, if Nadal’s stem cell treatment is being used to eliminate his pain by repairing his joints or discs, the actual cause of his back pain may not be addressed.
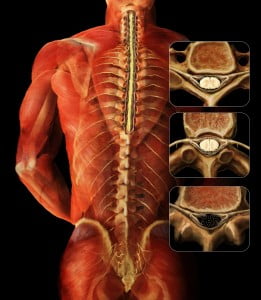
Where does back pain originate?
The number one reason for back pain is muscular and other soft tissue, yet muscles are rarely evaluated as the cause of back pain. The only way to determine if Nadal’s back pain is from soft tissue and similar to most people with back pain would be a physical examination of Nadal’s back that included identifying possible muscles as the cause of his pain.
Some doctors believe that the disc, the cushion between the bones of the spine (the vertebra), is a major cause of back pain. They believe that surgeries to correct the flattening or herniation of the disc will decrease or eliminate back pain. Sometimes they are right, but they are just as likely to be wrong. The truth is that there is as high as a 50% failure rate for spine surgeries that were done to eliminate back pain thought to be related to disc problems. There are other joints in the spine that are thought to cause pain; one of them is the facet joint, which could also be a target for stem cell treatments.
When doctors rely on an MRI or CT scan to determine the source of the pain, the information obtained is often confusing. If a surgeon sees an abnormality on an MRI, he will often point to that abnormality as the cause of the pain; in my experience the abnormality found on an MRI or CT scan frequently is not the cause. In fact, if you randomly selected 100 people off the street, and perform an imaging scan, 40 may present with a herniated disc and have no pain and absolutely no awareness of their herniated disc; 70 may have degenerated (worn) discs with no pain, and a large number will have facet joint abnormalities. Therefore, finding an “abnormality” is more common than not. One, then, can deduce that the abnormality is more likely NOT the source of the pain. So treating the abnormality (with steroid injections, surgery, or stem cells) may therefore not relieve the pain.
Stem Cell Treatment and Sports Stars
Nadal, currently ranked as the number 3 professional tennis player in the world, is not the first sports star to chase after a “miracle cure.” The Denver Bronco quarterback Payton Manning and Yankees pitcher Bartolo Colon both went abroad to seek out stem cell treatment as a quick fix to get back in the game. (They both seem to be doing better overall, but it is inconclusive if the stem cell treatment was the cause of their recovery).
Will it work?
In the laboratory, it has been possible to demonstrate the ability of stem cells (most commonly found in the developing embryo and newborn) to grow new tissue. These cells are like silly putty; they can turn into, or adapt, to become any type of tissue. For example, a stem cell in the right environment in the body could become bone, cartilage or some organ (for example, liver or pancreas). But, it hasn’t been as easy to grow tissue in an actual person. There are some early studies that show that stem cells “may” relieve back pain, but both the doctors who are testing the technique and outside experts say much more research is needed before they can say whether the treatment offers real relief.
The use of stem cell therapies continues to be a hot topic for debate in the sports medicine and orthopedic surgery worlds. There is no current evidence-based research to prove that it works.
Sir William Osler, a famous physician, once said: “Use every new treatment as quickly as possible before it stops working.” Stem cell treatment needs to be further investigated to determine if stem cell treatments indeed work, and if so, for what conditions?
Medical Mystery
For seven years, searing pain with no relief – that was the title of The Washington Post story that peaked my interest. So I read the article and discovered that Charon Wicker had been experiencing a burning, throbbing, excruciatingly painful sensation in her index finger – for seven years – even though she had:
- Repeatedly consulted pain specialists and orthopedic surgeons, internist and endocrinologist; and even a hand surgeon;
- Undergone two operations to replace the herniated disks in her neck;
- Taken all sorts of painkillers and become dependent on the sleeping pill Ambien;
- Received X-rays, MRI scans, and a nerve conduction test all negative);
- Spent months in physical therapy;
- Took a variety of anti-inflammatory drugs, increasingly strong painkillers, including oxycodone.
But nothing worked. Ms. Wicker’s pain continued.
The Case of Sore Fingertip looked as if it was a case for Sherlock Holmes (or his creator Dr. Arthur Conan Doyle) or Dr Gregory House.
It made me think — Be careful whom you ask for help!
And finally, Charon did get the right help from a hand surgeon who, listened to his patient; reviewed her medical history; and then examined her fingertip – where she had been complaining of pain for seven years, carefully. He saw a “slight bluish discoloration underneath her nail,” and found the cause of her pain — a rare benign vascular growth – smaller than the head of a pin – a tumor. He removed the glomus tumor and the pain was gone.
It’s uncommon to find that persistent pain is caused by a glomus tumor – but it is common that someone with persistent pain will be offered spine surgery to help them.
It is unfortunate that in Ms. Wicker’s case, she underwent TWO aggressive spinal surgeries and the pain continued. Even though her pain was in her fingertip (something that would clearly not be caused by a faulty disk or helped with insertion of an artificial disc in her neck) and there were no signs or symptoms that pointed to spine surgery to mitigate the pain, surgeons suggested two separate operations to replace the spinal disks. Whereas drugs have to go through extensive testing to show they are safe and effective, surgical procedures do not. When the first surgery didn’t work, the suggested solution was another surgery to replace another the disc.
In my practice, I have seen many patients over the years who come to my office complaining of chronic neck, shoulder, low back and/or leg pain that continues after “failed back spinal surgery. The herniated disc that was discovered on an MRI didn’t explain the source of their pain.
MRIs can show doctors beautiful pictures of the bones and the material separating the bones (the discs) of our spines but interestingly an MRI of the spine will usually find some “abnormality” in most adults – the majority of the time without any pain complaint. Desperation is often one of the reasons that patients undergo very invasive procedures based on an MRI and not supported by the clinical picture.
Sometimes a surgery works but how could it in The Case of Sore Fingertip? It didn’t and as Sherlock would say, “It’s elementary, my dear Watson.” It just didn’t make sense.
You can read the article in full here.
Men, Women, and Children — Simple Solutions to Eliminate Back Pain
Men:
Where do you keep your wallet? Many of you probably answered, “your back pocket.” Did you know that this could be causing your back pain?
When you sit down with your wallet in your back pocket, it presses into your muscles, which can cause pain in your low back and buttock. The squeezed muscle can press your sciatic nerve causing the pain to travel down your leg.
If you’re suffering from back pain, try keeping your wallet in an external bag or a front pocket. Or simply decrease the thickness of your wallet by taking out any extraneous items, such as old receipts or credit cards that you no longer need or use.
Women:
Those fashionable Jimmy Choos or Manolo Blahnik’s, which are known for their height, may actually be increasing your low back pain. But don’t switch out those high heels for the increasingly popular ballet flats or stylish sandals because flats can stretch and strain the muscles in the calves and thighs causing pain in the buttock and low back.
You don’t have to forgo fashion for comfort. Wearing low, comfortable heels can save your back from unnecessary pain. Remember to wear shoes that fit properly as well – ill-fitting shoes can cause you to tighten your leg and buttock muscles causing low back, buttock, and leg pain.
Children:
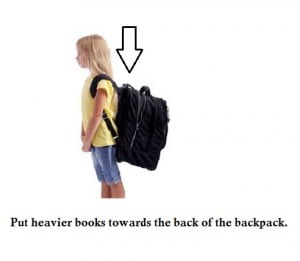
Now that school is back in session, many kids are carrying heavy books in their backpacks. Often, the heavy, incorrectly worn backpacks can cause poor posture and strain on muscles. Parents, have your child(ren) pack their backpacks so that the heaviest books are placed towards the back of the bag. This way, the heaviest part of the bag is closer to the back of the child. (see picture) Also, remind your child(ren) to use both straps on both shoulders. This helps distribute the weight evenly, as opposed to placing strain on one shoulder. Another option is using backpacks with rolling capabilities.
Similarly, all you ladies who stuff your shoulder bags with everything from lipstick to workout weights, carrying a heavy bag on your shoulder every day can be the source of your aching neck and back. While those oversize totes conveniently contain everything you might possibly need in a day, the accumulated stress on your neck and spine from “pocketbook overload” can lead to serious strain on your muscles, tendons, nerves, and ligaments, causing serious body aches. So what does a fashionable woman on the go do?
- If you absolutely must carry a tote, lighten the load – try to take out the items you don’t really use or need.
- Switch the bag from one shoulder to the other often, minimizing the amount of time you strain the shoulder and neck muscles.
- Try using two lighter bags instead of one big one. Splitting the load and carrying them on both sides distributes the weight evenly.
And don’t forget; no matter what you carry, having good posture helps reduce back pain.
Parents:
Lifting your baby 50 times per day, or bending and lifting up to get your active toddler out of his/her sibling’s hair, are innocent movements that can indeed cause low back pain. Good posture and proper lifting techniques can help parents avoid the increased risk for low back pain. Some key pointers:
- Keep your feet (shoulder width) apart, your back straight and bend your knees to reach for your child.
- Use your leg muscles, which are bigger and stronger than your back muscles, to lift your child. After you bend over, bring your child to your chest, bring your back to the upright position, and then straighten your legs. If you straighten your legs before bringing your body upright, you’re using your low back muscles to lift your child. However, if you straighten your legs last, then you’re using your leg muscles.
Keep in mind; this is a good tip for lifting anything heavy!
Eating forbidden foods, losing weight and helping your heart
I had dinner with Dr. Robert Atkins years before his untimely death. He ordered a juicy marbleized steak with a baked potato drowning in butter and sour cream. At the time I thought this wasn’t a healthy choice- I was wrong! A front page article in the NY Times earlier this week reports on a large year-long NIH funded study published in the Annals of Internal Medicine supporting the ideas of Dr. Atkins, viz. high fat/ low carbohydrate diets are better for your health than equal calories of high carbohydrate/ low fat diets. You not only lose more weight but your total cholesterol goes down and the good cholesterol (HDLs) goes up. This is a great example of showing us that what we firmly believe to be the truth (i.e. a low fat diet is best for your diet and health) may not be so. An important issue in this study is that both groups lost weight. Calorie restriction does work to lose weight- but it may be easier for some patients who have difficulty dieting, to limit their carbohydrates, still feel satisfied, and lose weight.
 As I report in my book End Back Pain Forever, a previous NIH funded study also showed that calorie reduction consistently resulted in weight loss; this new study reaffirms that low carbohydrate/high fat diets are healthier for your heart. In my book I reported that eating plant rather than animal protein/fat was preferable if you were concerned about lowering levels of the bad cholesterol (low density lipoproteins-LDLs). If you’re thinking of becoming a vegetarian- eating a vegetarian diet has been shown to produce the lowest levels of cholesterol and in general to be associated with the lowest BMIs (Body Mass Index, which is a measure of body fat based on weight and height.). The carbohydrates that are most damaging are refined carbohydrates such as found in white flour and sugar. No matter what diet you choose you need to get the minimal amounts of essential minerals and vitamins, therefore always include healthy amounts of fresh fruits and vegetables.
As I report in my book End Back Pain Forever, a previous NIH funded study also showed that calorie reduction consistently resulted in weight loss; this new study reaffirms that low carbohydrate/high fat diets are healthier for your heart. In my book I reported that eating plant rather than animal protein/fat was preferable if you were concerned about lowering levels of the bad cholesterol (low density lipoproteins-LDLs). If you’re thinking of becoming a vegetarian- eating a vegetarian diet has been shown to produce the lowest levels of cholesterol and in general to be associated with the lowest BMIs (Body Mass Index, which is a measure of body fat based on weight and height.). The carbohydrates that are most damaging are refined carbohydrates such as found in white flour and sugar. No matter what diet you choose you need to get the minimal amounts of essential minerals and vitamins, therefore always include healthy amounts of fresh fruits and vegetables.
To paraphrase Mark Twain, it’s very easy to diet and lose weight- I’ve done it twenty times; The trick is to keep it off once you’ve lost it. Here are some tips from my book:
1. Increase your physical activity. If you never walk anywhere, start to do that. If you walk two blocks a day, increase it to four. If you go to the gym once a week, increase it to twice a week. The idea is to begin where you are now and increase slowly and steadily. Don’t take on more than you can handle, but work your way up. Make yourself a winner by taking on an achievable goal.
2. Don’t attempt total deprivation. Avoid starvation diets. Your body senses that you are starving, and it adjusts by slowing your metabolism, the rate at which calories are burned. This makes it harder to lose weight. Being able to lose weight and maintain the loss requires changing the way you eat and increasing physical activity. Just as you changed your activity level gradually, do the same with diet. In other words, start slowly. Make one simple change. I recommend to my patients that they stop eating bread and pastries. Some love bread and can’t imagine living without it. They soon learn, though, that after a short while, the craving for bread diminishes and their weight starts to drop. Then stop eating pasta or only allow it (and bread) as a treat; let’s say on Sundays.
3. Learn how many calories are in the food that you eat. When patients tell me that all they eat is salad, but they’re gaining weight, I have to remind them that any sauce or dressing may contain high-calorie ingredients. When you are out at a restaurant, it is best to avoid foods that may hide unwanted calories.
Is Bad Weather To Blame For Your Lower Back Pain?
A New York Times article Weather May Not Affect Back Pain, printed mid-July, cited a study showing that weather may not affect back pain. The purpose of the study was to explore the often-heard complaint from patients diagnosed with persistent pain related to muscles and bones (musculoskeletal pain) that weather changes cause an increase in pain. The study was based on an analysis of 993 patients who had seen their physician in 2011-2012 complaining of an episode of sudden back pain. These were not patients with a history of back pain.
So this article does not actually examine patients who already have back pain to see if the pain is increased with bad weather. In my practice, at NMPI, I have patients who can tell me a snowstorm is coming 3 days before it occurs. Although studies of the association between weather and pain are not uniformly supportive of the connection, a study done in 1995 of 558 patients with chronic pain found that 2/3 experienced an increase in pain and most of them prior to the occurrence of the bad weather.
 I have patients whose pain is so severe with bad weather that they can hardly get out of bed. Although there is no good scientific explanation for this association, some suggestions have been offered. When the barometric pressure falls, the air pressure in a painful joint may continue to be a little higher than the air pressure on the outside of the body, causing an increase in pain. Another explanation is that cold and/or inclement weather decreases the amount of time you are outside and active. Patients with musculoskeletal problems (i.e. muscle pain and arthritis) often feel worse with inactivity. In addition cold weather causes the blood vessels in the hands and feet to constrict, which can decrease the amount of available oxygen, resulting in increased muscle pain.
I have patients whose pain is so severe with bad weather that they can hardly get out of bed. Although there is no good scientific explanation for this association, some suggestions have been offered. When the barometric pressure falls, the air pressure in a painful joint may continue to be a little higher than the air pressure on the outside of the body, causing an increase in pain. Another explanation is that cold and/or inclement weather decreases the amount of time you are outside and active. Patients with musculoskeletal problems (i.e. muscle pain and arthritis) often feel worse with inactivity. In addition cold weather causes the blood vessels in the hands and feet to constrict, which can decrease the amount of available oxygen, resulting in increased muscle pain.
If your history indicates that bad weather causes an increase in your pain, it is likely that your flare up is most likely not an indicator of physical deterioration. Additional pain can be reasonably treated with increased medication for the brief period of weather related pain.
49 States Adopt Prescription Drug Database to Prevent Prescription Drug Abuse
Because of the growing problem of addiction, misuse, and diversion, 49 states have now adopted a state prescription drug database. You may have read an article recently in The New York Times about Missouri being the only state that has not adopted such a database. In New York, as a prescriber of controlled substances, each time a patient is prescribed any type of controlled substance, I must log into the NYS website to confirm that a patient is not receiving other medications from other doctors.
 I found a few patients who had not been honest with me and had received medications from other doctors. Unfortunately, the small occurrence of dishonest behavior has obliged all doctors to be alert for the possible misuse of medication. At the Norman Marcus Pain Institute, I implement several rules for patients receiving any type of controlled substance from me. Here are a few of them:
I found a few patients who had not been honest with me and had received medications from other doctors. Unfortunately, the small occurrence of dishonest behavior has obliged all doctors to be alert for the possible misuse of medication. At the Norman Marcus Pain Institute, I implement several rules for patients receiving any type of controlled substance from me. Here are a few of them:
• Only one physician can prescribe all pain medications.
• Only one pharmacy should be used to obtain all pain related medications.
• All medications, including herbal remedies and over the counter medications, need to be reported since all medications can interact with one another.
• Medications must be kept in a safe and secure place, such as a locked cabinet or safe.
Following these simple rules will help protect my patients and their families from improper use of pain medication.
Concerns about the Growing Misuse of Opioids – Prescription Painkillers
From 1991 to 2009, the number of prescriptions written for the strongest pain medications tripled. These medications are collectively named opioids and include morphine, oxycodone, and hydrocodone.Opioids are a type of pain drug that may cause serious side effects. From 2005 to 2009, the number of emergency room visits for nonmedical use of prescribed pain medication doubled. Therefore, the states and federal governments are acting to try to limit the amount of pain medication being prescribed.
At NMPI, we focus on finding the most effective treatment to relieve our patients’ pain – without surgery, steroid injections, or heavy painkillers. However, when a patient complains of severe pain and is not responding well to other pain medications, stronger, prescription opioids will be given.
 Some opioids, such as oxycodone, are often combined with Tylenol (acetaminophen) in one pill. Some examples of these combination drugs are Lorcet, Lortab, Norco, Vicodin (are all hydrocodone and acetaminophen), and Percocet (oxycodone and acetaminophen). Most often, severe pain is related to a condition that will improve over time. Ideally, all prescription pain medications should be given only while severe pain persists. Like any medication, there are risks and side effects:
Some opioids, such as oxycodone, are often combined with Tylenol (acetaminophen) in one pill. Some examples of these combination drugs are Lorcet, Lortab, Norco, Vicodin (are all hydrocodone and acetaminophen), and Percocet (oxycodone and acetaminophen). Most often, severe pain is related to a condition that will improve over time. Ideally, all prescription pain medications should be given only while severe pain persists. Like any medication, there are risks and side effects:
• Opioids can make you drowsy – which raises the risk of falling and severe injury
• Opioids when mixed with alcohol, anti-anxiety medication, seizure medication, muscle relaxants, or sleep-aids can be deadly.
• Opioids cause constipation and can lower sex drive.
• Patients can become physically and psychologically dependent on opioids.
• Overtime a patient with chronic pain can develop a tolerance for the opioid and need a higher dosage.
Keep in mind that not all pain requires such strong medication, and most patients with pain can be managed with drugs such as acetaminophen (Tylenol) and aspirin-like drugs, called non-steroidal anti-inflammatory drugs (such as ibuprofen and Naproxen). When taken as directed, these less powerful drugs may be all that you need. (There are potential serious side effects with acetaminophen and NSAIDs, which I will discuss in a future blog.) For certain pains, some drugs are better than others. Sometimes we find that a drug we have been using may not actually be effective. A New York Times article on July 23, 2014 reported that for treating low back pain, acetaminophen was no better than a placebo.
Physicians have a responsibility to properly care for patients in pain. Some of these patients may appear to be at a higher risk to abuse opioids. Occasionally, patients complain of non-existent pain to obtain opioids for its mood-altering affect, called a “high.” The fact is that physicians who had been writing too many prescriptions for pain medication are now wary of prescribing any potentially habit-forming pain drugs. This has resulted in a decrease in emergency room visits for drug overdose and deaths from overdose, but it has also resulted in depriving many patients of medication they legitimately need to function normally.
At NMPI, when we treat patients in pain who have a history of drug abuse or who test positive on a written test to determine the risk of abuse, I believe that these two basic American traditions should be the guiding principles:
1. Innocent until proven guilty; and
2. In the words of Ronald Reagan, Trust but verify. Those patients who have problems or are at risk to not properly use pain medication need extra attention, not condemnation. They may be more difficult to treat, but that is why there are specialists to deal with complex pain problems.
Morphine: Friend or Enemy?
You may have read several articles in the news lately about opioids and pain medications. Earlier in July, The New York Times printed two separate articles on the dangers and abuse of prescriptions drugs in the States. On July 1st, Sabrina Tavernise’s Prescription Overdose Deaths in Florida Plunge After Tough Measures, Report Says, appeared in the Health section and on July 3rd, The Op-Ed editors wrote a piece entitled States and Painkiller Overdoses.
Obviously, the media is very concerned regarding the large number of pain medications being prescribed, the amount of medications being misused and/or diverted, and the adverse effects of the medication, particularly addiction.
Back in the day, alcohol was used as anesthesia for surgeries – patients were given a bottle of bourbon and told to bite the bullet. Modern medicine introduced Ether and chloroform for surgical procedures and morphine to control the pain after the surgery. Morphine was thought to only be effective by injection, but then we found that morphine tablets and liquid taken by mouth could be just as effective in relieving pain. Morphine was then used for patients with terminal cancer pain. Why not make a dying patient comfortable?
The availability of oral instead of injectable morphine allowed doctors caring for cancer patients to more easily relieve the suffering that many dying cancer patients experienced. If it was good for cancer pain, why not use it for back pain and neck pain? Short acting and long acting morphine-like drugs were developed and a new approach to pain control became the standard of care. Use morphine and other related drugs, such as oxycodone, Oxycontin, Dilaudid, and hydrocodone, and if the patient has more pain, raise the dose of pain medication.
Although overdose could interfere with breathing and cause death, the most troublesome side effect with careful use was thought to be constipation. Other adverse effects of these medications began to be observed, such as addiction and opioid-induced hyperalgesia (when the morphine-like pain medication actually causes more pain).
In addition, people who had been using mind-altering drugs like heroin recognized that they could get the same effect from prescribed medications, which could be cleaner and cheaper. The illicit use of prescription pain drugs is a growing problem in the USA, and are actually the preferred street drug after marijuana.
At NMPI, we only use prescription drugs like oxycodone, Oxycontin, Dilaudid, and hydrocodone to relieve severe pain when patients are unresponsive to our usual therapies. We take a holistic approach to the treatment of pain. Our treatments include:
- Exercises
- Muscle/tendon injections (no cortisone or any other steroids are ever injected into the muscle tissue)
- Low-level laser therapy, which can aide in the healing of damaged muscle tissue and sensitized fibers found in the muscle attachments.
- Traditional and novel medications, relaxation therapy, and counseling
In the next few blogs, I will discuss the problems arising with prescription drugs for pain relief and what steps are being taken to try to manage this problem.
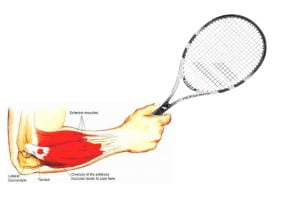
Tennis Elbow Causing You Pain? PRP is NOT the Solution Study Shows
At NMPI, we frequently see patients in our office with pain in their elbow. Most often it’s tennis players who complain of persistent pain in the forearm as the result of overuse from racquet sports but other sports and non-athletic activities can also put you at risk for this condition known as Tennis Elbow (TE), or lateral epicondylitis. Strain related changes in the tendons that join the forearm muscles to the outside of the elbow can be very painful.
I was not surprised to read in the British Journal of Sports Medicine, that a recent study (Strong Evidence Against Platelet-rich Plasma Injections for Chronic Lateral Epicondylar Tendinopathy: A Systematic Review) reported that PRP, which I recently reported as not being effective for hamstring injuries, is now found to be ineffective for persistent Tennis Elbow as well. PRP has been increasingly used for many painful conditions that athletes experience. This is based on the finding that in laboratory animals healing can be induced in damaged tissue if platelets are injected into the injured area. The popularity of PRP for TE has grown despite no strong evidence that it actually works. Sir William Osler, a renowned physician once said “use every new treatment as quickly as possible before it stops working.” At NMPI, we do not rush to use a “new” approach just because it is new. We are committed to eliminating our patients’ pain and preventing its recurrence.
TE is commonly diagnosed by producing pain when pressing on the tendons that attach to the lateral epicondyle along with pain when the wrist is pulled upward (dorsiflexion) against resistance. TE is generally self-limiting but in some patients it may take more than a year to get better with no treatment. When the pain and tenderness persist various treatments have been tried.
Here’s what works:
- In a 2010 paper, an exercise treatment was found to be very effective in relieving TE pain and tenderness.
- At NMPI, we treat these tender muscles successfully with a laser or with muscle injections.
Here’s what doesn’t work:
- Steroids are not recommended since there is no inflammation in TE and steroids can actually damage the tendon.
- PRP for tennis elbow has been found to not be effective
Newer treatments are often not better. It is always best to first treat any lasting pain problem with the least invasive, safest, and least expensive interventions. This is called the step-care model and the approach you will receive at the Norman Marcus Pain Institute.
Platelet Rich Plasma Injections (PRP) are not effective for Hamstring injuries
PRP injections have become a frequently used treatment for painful muscle and tendon injuries despite there being no rigorous studies of its effectiveness[1]. PRP involves the drawing of blood from the injured patient, spinning it down to collect the platelets and then injecting the platelets into the injured tissue. The rationale is that platelets will provide growth factors that will make you heal faster.
A study[2] reported on in a letter to the New England Journal of Medicine found that athletes with hamstring injuries recovered no better with PRP than with placebo (a salt water injection). In a randomized double blind controlled study (RCT), in which 80 recreational and professional athletes with hamstring injuries received either PRP or placebo injections, there was no difference in the average amount of time it took for each group to return to normal activities. In other words, in this study, injections with salt water were as effective as the $1600 injection of platelets. It is often difficult to treat pain related to muscles and tendons. For anyone in pain, a suggested treatment that can get you better faster and is offered by respected physicians is hard to resist. The problem is that without carefully studying a new procedure, compared to a similar control treatment, it is not possible to be sure that the new treatment actually works better. This first RCT of PRP for hamstring injuries suggests that it may not be a reasonable approach to painful muscle injuries.
If the assessme nt of muscle pain was a routine part of the physical examination, time, money and suffering could be minimized. At the Norman Marcus Pain Institute, our approach to painful muscles following injury is based on the work of my mentor, Hans Kraus, M.D., President JFK’s physician for the treatment of his back pain. Painful muscles are frequently the result of tension, weakness, stiffness, spasm or altered muscle tissue (usually referred to as trigger points).
nt of muscle pain was a routine part of the physical examination, time, money and suffering could be minimized. At the Norman Marcus Pain Institute, our approach to painful muscles following injury is based on the work of my mentor, Hans Kraus, M.D., President JFK’s physician for the treatment of his back pain. Painful muscles are frequently the result of tension, weakness, stiffness, spasm or altered muscle tissue (usually referred to as trigger points).
At the Norman Marcus Pain Institute, our physical examination tests for all these causes of pain so that the simplest cost effective treatments can be provided prior to using any invasive procedures. Sometimes severe pain is quickly eliminated with our exercise, electrical stimulation and laser protocols that are described in detail in my book End Back Pain Forever. Your pain may require medication and injections, because one size does not fit all.
[1] Moraes VY, Lenza M, Tamoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2013.
[2] Reurink G, Goudswaard GJ, et al. Platelet-Rich Plasma Injections in Acute Muscle Injury. N Engl J Med. 2014:370:2546-2547.
Epidural steroids are not effective for spinal stenosis
I have been suggesting for many years that there is an overuse of spinal injections and surgeries for low back and leg pain, so it was no surprise when I read an article in The New York Times (NYT) that reported on a study recently published in the New England Journal of Medicine[1] about patients with spinal stenosis who are frequently treated with a procedure that has been shown to be ineffective. Epidural steroid and lidocaine injections for patients found to have spinal stenosis were no better than epidural injections of lidocaine alone. In chapter 4 of my book End Back Pain Forever I discuss the many reasons for back pain. MRIs and CT scans of the low back will almost always find something such as spinal stenosis or a degenerated or herniated disc even in patients without pain. Therefore the US Institute of Medicine suggests that these imaging studies should not be done routinely since what you find in the study is frequently not the cause of your pain. The most common cause of back pain is muscles and other soft tissue. If you treat the diagnosis you got from the MRI or CT and the actual reason for the pain is muscle, it makes sense that the treatment will frequently fail, which it does!
The NYT report of this relatively large, randomized, double blind, controlled study clearly demonstrates the ineffectiveness of the use of steroids for symptoms attributable to spinal stenosis (narrowing of the canal in the spine which contains the spinal cord) which occurs frequently as we age. The treatments most often provided are epidural steroids to theoretically reduce the inflammation of the nerves being squeezed by the narrow canal, and surgery to widen the canal. Both approaches have a significant failure rate.
At the Norman Marcus Pain Institute we have shown in multiple published articles that one reason why these approaches are ineffective is that the pain in the back and leg may not be the result of the narrowing or other supposed abnormalities seen on the MRI or CT scan. It is well known that very few (in one published article- less than 10%) scans of the low back in adults are read as normal; as many as 40% of adults with no back pain have herniated discs, and 70% have degenerated discs. So it is “normal” to find an abnormality.
Our unique physical examination, utilizes an instrument I developed, reveals that many patients with back and leg pains have areas of muscle tenderness that are the source of their pain yet are overlooked. One study of more than 23,000 patients[2] found that 70-80% of patients with back pain were diagnosed with sprains and strains of muscle and other soft tissue. It’s hard to believe then, armed with this knowledge, that muscle examination and treatment is not part of the typical standard of care for back pain in the USA[3]. If we are to properly address the cause of most back pain, the evaluation and treatment of its muscular causes must be addressed.
[1] Friedly JL, Comstock BA, Turner JA, et al. A Randomized Trial of Epidural Glucocorticoid Injections for Spinal Stenosis. New England Journal of Medicine. 2014:374:11-21.
[2] Deyo RA, Weinstein JN. Primary care – low back pain. New England Journal of Medicine. 2001:5:363-70.
[3] Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, et al. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
Sometimes the pain isn’t coming from where you think
I recently saw Fred, a 30 year old male, who complained of significant neck pain and shoulder pain. The pain on his left side was much greater than on the right. He tried several chiropractic treatments, massage, physical therapy, acupuncture, and exercises without relief of his pain.
When I first examined Fred, I found two muscles that were painful, his anterior and medial scalenes on both sides. The scalenes are muscles that go from the side of the neck down to the 1st rib as it sits under the clavicle (collarbone). Since he complained mostly of pain on his left neck and shoulder, I injected his left scalenes, followed by 3 days of physical therapy (which included neuromuscular electrical stimulation and gentle, limbering exercises). Fred claimed that the pain on the left subsided, but he noticed that the right side was now more painful. So, the following week, he had his right scalenes treated (with injections into the muscle, followed by 3 days of physical therapy). Fred reported a significant decrease in his overall pain, and reported only soreness at the injection sites.
I followed up with Fred approximately one month later. He reported to me that his overall pain level continued to stay low, but he noticed that when he looked up, he felt tightness on the left side of his neck. When I examined him, I found two muscles to be contributing to his pain, the Serratus Anterior and the Subscapularis. These muscles are in his shoulder. He was very shocked to learn that tightness in his neck was caused by muscles in his shoulder!!
Once these muscles were treated, he reported that the tightness in his neck was released. Sometimes we have to look for muscles contributing to pain in areas other than where you may be feeling it. This is called referred pain. If I had continued to treat muscles in Fred’s neck, he may never have had relief!
Stiffness is an important aspect of muscle pain
I recently saw George, a 48-year-old man, who suffered from pain, described as soreness in the thighs, neck, shoulders and arms, and tingling in his calves and shin. Sitting for more than two hours or sitting for more than 20 minutes would cause an increase in his pain. Bending over also brought on his pain.
George had tried physical therapy on multiple occasions, and saw two neurologists, who could not find anything that would explain his pain.
When I examined him, I found him to be strong but very stiff. When he bent over, he was able to reach within 14 inches of the floor. When he lied on his back and lifted one leg up at a time, he was able to reach only 57 degrees (85 75 degrees is normal). Because he was so stiff, I decided to start a course of exercises that would help increase his range of motion.
Over the next few weeks, George learned all 21 of the Kraus-Marcus exercises, which he was advised to do every day. As he did the exercises, he noticed that his pain level was decreasing and wasn’t occurring as often as usual. When he was taught the last 7 exercises, he was able to bend over to within 9 inches of the floor, and could lift each leg to 80 degrees.
A month later, George reports a 90% decrease in his overall pain. Sometimes we find that starting with the most conservative of treatments can prevent us from performing more costly and dangerous treatments. Very often, stiffness is an important aspect of one’s pain that can easily be found and treated!
Low Level Laser Therapy as promising treatment
Low level laser therapy (LLLT) is a promising new treatment for a variety of painful conditions which is believed to reduce inflammation and stimulate healing of wounds. Interest in the laser first developed when Endre Mester at Semmelweis University noticed that applying the laser to the backs of shaven mice caused hair to regrow faster than those who did not receive laser treatment.[1] This observation prompted further study into the regenerative effects of the laser first in rats, and then later in humans.
Currently, there aren’t many large-scale studies evaluating the effectiveness of the laser, but smaller studies of the laser for painful conditions show promising results.
A study of 50 patients with knee osteoarthritis reported that the laser was significantly more effective at providing pain relief than transcutaneous electric nerve stimulation (TENS)**.[2] Similarly, a separate study of 125 patients with knee osteoarthritis reported both an improvement in pain and an increase in function after LLLT.[3]
In a study of patients with temporomandibular disorders, the laser improved pain within 24 hours, with relief lasting at the 180 day follow-up.[4]
Current studies show that the laser is an up and coming, non-invasive, non-painful treatment option, but larger studies are needed to determine the correct dosing, and for which conditions the laser will be most useful.
**TENS (transcutaneous electrical stimulation) – electrodes are applied to the skin, sending an electric current to the nerves in the skin. The nerves then transmit a signal to the brain. This signal is competing with the signal coming from your painful area. So, instead of feeling your normal pain, you’ll feel a buzzing sensation where the electrodes are attached.
[1] Chung, Hoon, Tianhong Dai, Sulbha K. Sharma, Ying-Ying Huang, James D. Carroll, and Michael R. Hamblin. “The Nuts and Bolts of Low-level Laser (Light) Therapy.” Annals of Biomedical Engineering 40.2 (2012): 516-33. Print.
[2] Kędzierski, Tomasz, Katarzyna Stańczak, Kamila Gworys, Jowita Gasztych, Marcin Sibiński, and Jolanta Kujawa. “Comparative Evaluation of the Direct Analgesic Efficacy of Selected Physiotherapeutic Methods in Subjects with Knee Joint Degenerative Disease – Preliminary Report.” Ortopedia Traumatologia Rehabilitacja 14.6 (2012): 1-10. Print.
[3] Gworys, Kamila, Jowita Gasztych, Anna Puzder, Przemysław Gworys, and Jolanta Kujawa. “Influence of Various Laser Therapy Methods on Knee Joint Pain and Function in Patients with Knee Osteoarthritis.” Ortopedia Traumatologia Rehabilitacja 14.3 (2012): 269-77. Print.
[4] Pereira, T. S., O. D. Flecha, R. C. Guimaraes, A. M. Botelho, JC Ramos Gloria, and K. T. Aguiar Tavano. “Efficacy of Red and Infrared Lasers in Treatment of Temporomandibular Disorders–a Double-blind, Randomized, Parallel Clinical Trial.” Cranio : The Journal of Craniomandibular Practice 32.1 (2014): n. pag. Ovid. Web.
Small changes may make a big difference to your neck pain
There has been an increase in the number of hours we sit in front of a computer for leisure and work. Does your job require you to stare at a computer for hours at a time? One study found that workers sitting for 95% of the day, and/or worked with their neck at 20˚ or more in flexion for more than 70% of their working time, had a significantly increased risk of neck pain[1].
An ergonomically designed workstation would help reduce the strain on your muscles. Here are a few suggestions:
- Place your monitor so you are looking at it straight ahead or down at no more than a 15˚ angle.
- The monitor should be 18-24 inches away.
- The angle of your elbows when typing on the keyboard should be > 90 degrees.
- An ergonomic mouse or keyboard may also help.
- A laptop is always non-ergonomic; because the monitor and keyboard cannot be separated one or the other is in the wrong position. If you always use a laptop think about getting an auxiliary keyboard.
- Footrests should be used if your feet do not rest flat on the floor.
- If you use a phone frequently get a headset so you will not have to hold the handset to your ear.
Aside from these changes, you may also consider doing limbering activities such as small stretches throughout the day – shrug your shoulders a few times, move your arms above your head, or get up and walk around your chair.
[1] Ariens, G. AM, P. M. Bongers, M. Douwes, M. C. Miedema, W. E. Hoogendoorn, G. Van Der Wal, L. M. Bouter, and W. Van Mechelen. “Are Neck Flexion, Neck Rotation, and Sitting at Work Risk Factors for Neck Pain? Results of a Prospective Cohort Study.” Occupational and Environmental Medicine 58 (2001): 200-07. BMJ Group. Web.